One thing is certain as California heads for a new health insurance era under the Affordable Health Care Act, better known as Obamacare:
Almost all parts of the state will need more medical professionals to serve the additional 2 million to 4 million newly insured Californians. Should they, could they, mostly be physicians, or should other health care professionals like pharmacists, optometrists and nurse practitioners do some things now in the exclusive realm of MDs?
An optometrist – Democratic state Sen. Ed Hernandez of West Covina – leads the effort to let non-doctors do more.
Would that be good or bad? Try this real-life situation: You need care for distorted vision in one eye. You go first to the local optometrist, someone who now mostly does things like eye exams (sometimes without dilation) and fitting of contact lenses.
You don’t know it, but a bleed in a small capillary atop the retina is causing the problem. It takes an advanced scan using a dye to determine this for sure and not even all MD ophthalmologists are equipped to perform that in their own offices.
Will more people with this problem lose vision while seeking care from someone not fully equipped to deal with the situation? Or, since optometrists are easier to find than MD ophthalmologists, will more people get treatment faster by going to them first and then being sent to an MD? Also, since optometrists are fully capable of diagnosing eye problems stemming from diabetes, high blood pressure and strokes, should they be allowed to prescribe drugs for those conditions?
You could ask similar questions about other symptoms and problems from early indications of cancer to ear infections, now often diagnosed by nurse practitioners.
Hernandez wants to let the state’s 16,000 licensed nurse practitioners (more highly trained than registered nurses) set up their own shops, not always supervised by MDs. But he says most would still be under the aegis of doctors via today’s array of health care networks. No doubt this could make care more accessible, but might it cause sophisticated diagnoses to be missed? There’s that question again: Does increased access for hundreds of thousands outweigh potential risks?
“Pharmacists are the most underused of all health professionals, considering their years of education and training,” Hernandez says. He would let them prescribe birth control pills and other types of medication, including vaccines. Would they know enough about patient medical histories to avoid errors? Would they, for instance, know which organ transplant recipients can receive vaccinations and what types? Pharmacists often give drug-related advice today, generally on over-the-counter products or after patients show up with a doctor’s scriptA. Hernandez believes the majority could handle much more.
He notes that only about one-third of medical school graduates go into family practice as primary, first-contact doctors. The rest become specialists. “I think we should let specialists handle the complex cases,” he said, noting that many doctors already have nurse practitioners performing routine tasks in their offices.
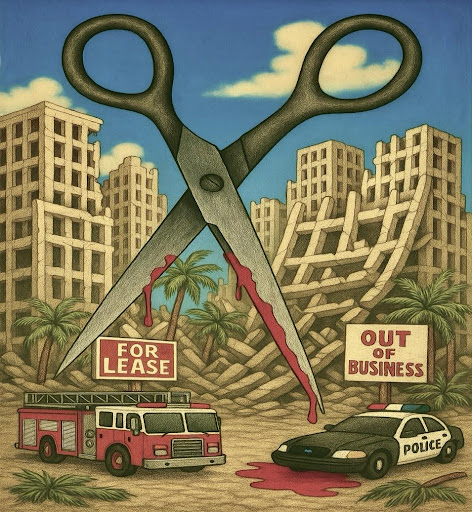
Behind this discussion lies that certainty of a coming doctor shortage. The California Medical Association (CMA) would like to see more medical schools added to University of California campuses, and that’s the long-term solution. But it would take years, and there would be more years for students to finish their studies and subsequent internships, residencies and fellowships.
Plus, there has been no great upsurge of documented medical errors in states that have expanded the scope of nurse practitioners’ work. Of course, delayed diagnoses and treatments don’t show up as errors.
Most doctors strongly oppose giving expanded privileges to any other health care professionals, even if Hernandez insists that no one would do anything they can’t do now. (For example, many pharmacies now give flu shots and the vast majority of patients with vision problems see optometrists first, anyway.)
The CMA is adamant that non-doctors performing clinical services have direct supervision and the ability to consult a physician quickly for problems beyond their ken. But even MDs have long forwarded difficult cases to specialists.
The bottom line is that something has to be done to make more professionals available to more patients, and do it in a way that fits the tight financial guidelines of Obamacare.
Some officials suggest giving incentives for doctors to bring more other professionals into their offices, combining ophthalmology with optometry, for example. Or using more nurse practitioners in internal medicine practices.
One thing for sure: Change is coming to health care because it’s coming to both health care pricing and health insurance. There’s already a battle to determine its shape.